Nurse Practitioner Collaborative Agreement Template
Streamline nurse practice collaboration with our template—clear agreements for seamless teamwork in healthcare. Download now!

By Joshua Napilay on Jul 15, 2024.
Fact Checked by RJ Gumban.

Table of content
What is a Nurse Practitioner Collaborative Agreement Template?
A Nurse Practitioner Collaborative Agreement Template is a legally binding document outlining the collaborative relationship between a Nurse Practitioner (NP) and a collaborating physician. New York State Education Law mandates this agreement to ensure patient care meets legal requirements and maintains high standards of practice.
The agreement defines the scope of the NP's practice authority and details the responsibilities of both parties in delivering patient care. This collaborative approach fosters a high-quality healthcare environment while adhering to legal mandates.
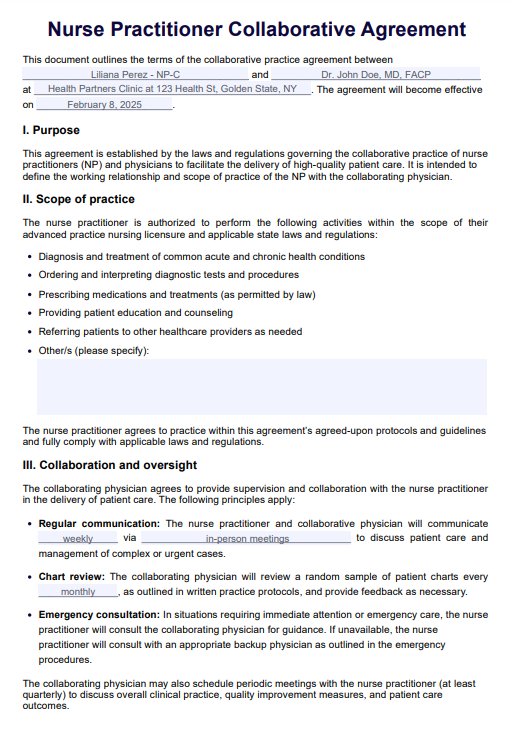
PDF Template
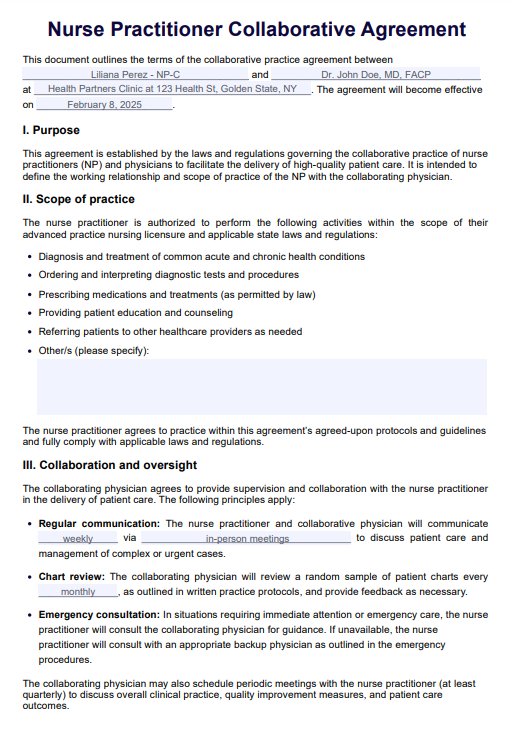
Example PDF
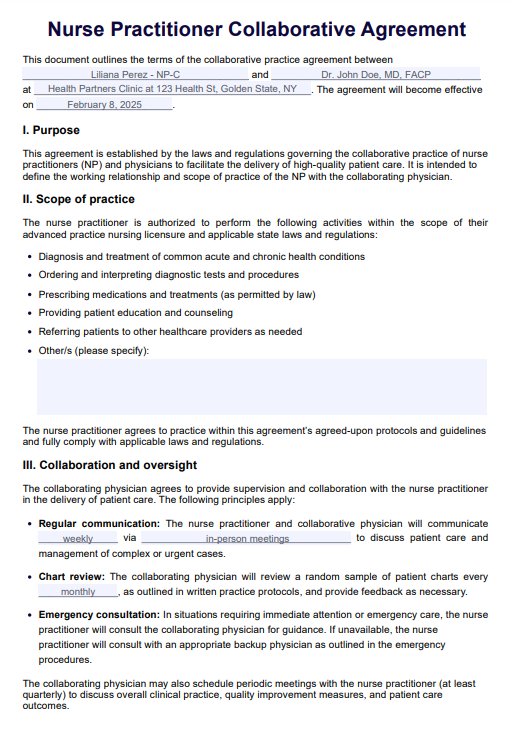
Nurse Practitioner Collaborative Agreement Template
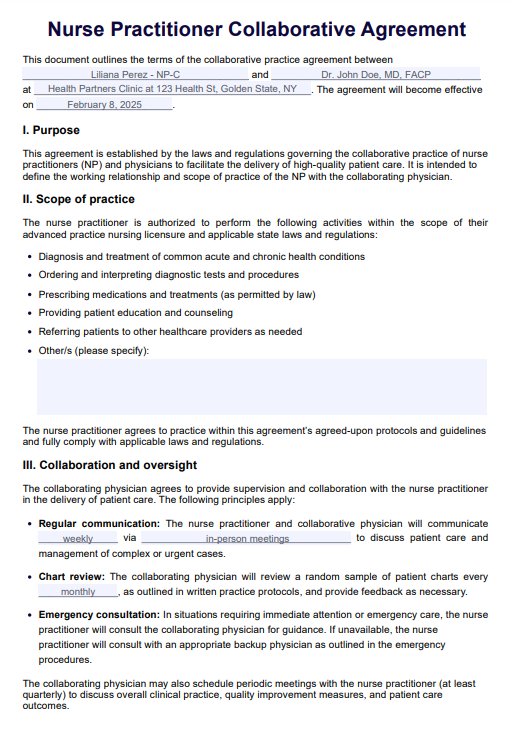
Nurse Practitioner Collaborative Agreement Template Example
Key elements of a Nurse Practitioner Collaborative Agreement Template
This section explores the essential components typically included in a Nurse Practitioner Collaborative Agreement Template:
- Parties involved: Identify the NP and the collaborating physician.
- Scope of practice: Defines the NP's authority for activities like diagnosis, treatment, tests, and medication prescription, all within the legal framework of New York State.
- Collaborative protocols: Details the written practice protocols the NP must follow as per state regulations.
- Patient care responsibilities: Specifies how patient care will be delivered, including consultation, referral, and follow-up procedures.
- Chart review & co-signatures: Outlines the collaborating physician's chart review process and any requirements for co-signing the NP's orders.
- Collaborative oversight: Describes how the physician will supervise the NP's practice, including communication and oversight methods.
- Dispute resolution: Establishes procedures for resolving disagreements or conflicts that may arise during collaboration.
- Record-keeping: Specifies how patient records will be created, maintained, and accessible for inspection.
- Review & updates: Includes a process for regular review and updates to the agreement to ensure compliance with evolving laws and practice changes.
- Signatures & date: Includes designated spaces for both parties to sign and date the agreement, signifying their commitment to collaborative patient care.
Remember: This guide provides a general overview. Consulting with legal counsel is crucial to ensure your agreement complies with all applicable New York State regulations.
Why nurse practitioners need collaborative agreements
Nurse practitioners (NPs) rely on collaborative agreements for several key reasons:
- Legal compliance: Many states, like New York, mandate these agreements to ensure NPs practice within legal boundaries. These agreements define the scope of practice for NPs, outlining what they can diagnose, treat, and prescribe independently or in collaboration with a physician.
- Patient safety: Collaboration fosters access to physician expertise for complex cases, enhancing patient safety through timely referrals, consultation, and shared decision-making.
- Quality of care: Collaborative agreements often establish protocols for communication, chart review, and quality assurance. This ongoing interaction promotes professional development and adherence to best practices.
- Continuity of care: Clear roles and responsibilities established in these agreements ensure smooth care coordination across healthcare settings and providers.
- Regulatory compliance: These agreements help NPs comply with regulations from licensing boards, professional associations, and healthcare institutions. Failure to have a valid agreement can lead to legal or disciplinary actions.
By fostering compliance, patient safety, and quality care, collaborative agreements form the foundation for a successful NP practice.
How does a collaborative agreement differ from a supervisory agreement?
Nurse practitioners (NPs) may encounter two agreements governing their practice: collaborative and supervisory. While both establish the relationship between an NP and a physician, they differ in crucial aspects:
Collaborative agreement
In a collaborative agreement, NPs and physicians work together as a team to deliver patient care. This fosters a more flexible and dynamic approach, allowing NPs to leverage their expertise while benefiting from physician guidance.
- NP autonomy: NPs have a defined scope of practice, allowing them to diagnose, treat, and manage patients independently within those parameters.
- Physician oversight: Collaboration involves physician guidance and consultation, not necessarily requiring physical presence during all encounters. The collaborating physician supports and ensures the NP stays within its legal boundaries.
- Agreement details: This agreement outlines specific roles and responsibilities for both parties, including communication protocols, record-keeping, and dispute-resolution mechanisms. A well-defined collaborative agreement streamlines communication and fosters a smooth working relationship.
Supervisory agreement
In a supervisory agreement, the physician takes a more direct role in overseeing the NP's practice. This approach is often used for newly licensed NPs or those working in complex specialties where closer guidance might be necessary.
- Limited NP autonomy: NPs may require physician approval or co-signatures for specific clinical decisions or actions. This ensures the NP benefits from the physician's experience and adheres to best practices.
- Physician involvement: Supervisory agreements often involve more direct physician involvement in patient care, such as conducting joint patient visits, reviewing all patient charts, and providing direct oversight of clinical activities. This allows for close monitoring and ongoing learning for the NP.
- Ongoing evaluation: These agreements often include provisions for continuing assessment and feedback from the supervising physician to the nurse practitioner. This feedback helps ensure the NP meets practice standards and regulatory requirements, promoting continuous improvement in patient care.
Choosing the right agreement
The type of agreement (collaborative or supervisory) depends on state regulations and the specific practice setting. NPs with advanced experience and expertise may opt for a collaborative agreement, while newly licensed NPs or those working in complex specialties may benefit from a supervisory agreement. Consulting with legal counsel and understanding your state's requirements is crucial for choosing the most appropriate agreement for your practice.
Can nurse practitioners practice without a collaborative agreement?
It depends on location and practice authority. The ability of nurse practitioners (NPs) to practice independently hinges on their state's regulations and the level of practice authority granted.
- Limited practice states: Many states mandate collaborative agreements with physicians. These agreements define the scope of practice for NPs, outlining what they can diagnose, treat, and prescribe independently or in collaboration with a physician.
- Full practice authority states: In contrast, some states grant NPs full practice authority, allowing them to practice independently without a collaborative agreement. NPs in these states may still choose to collaborate with physicians for specific cases, but it's not a legal requirement.
Regardless of location, NPs must be familiar with their practice's specific regulations. Operating outside these regulations, including failing to maintain a required collaborative agreement, can lead to legal repercussions.
Can a nurse practitioner have multiple collaborative agreements?
Yes, but know your state's rules. Nurse practitioners (NPs) can have multiple collaborative agreements with physicians or healthcare organizations in many locations. However, regulations for these agreements vary by state, so understanding your specific jurisdiction is crucial.
Here are some of the benefits of multiple agreements:
- Expanded practice: Collaborating with diverse physicians or organizations allows NPs to access broader practice settings and patient populations, enriching their experience and professional development.
- Flexibility: Multiple agreements offer scheduling and practice flexibility. NPs can work part-time or per diem with collaborators to suit their needs and goals.
- Continuity of care: Redundancy from multiple agreements ensures continuity of care for patients if a collaborating physician becomes unavailable.
- Diverse collaboration: Working with various healthcare professionals fosters valuable networking, knowledge sharing, and professional growth.
While beneficial, NPs must ensure compliance with all legal and regulatory requirements in each practice location. This includes:
- Limits on agreements: Understanding any limitations on the number of allowable agreements within your jurisdiction.
- Clear communication: Maintaining open communication and coordination between collaborating physicians or organizations to guarantee consistent, high-quality patient care.
Multiple collaborative agreements can be a strategic choice for NPs, offering expanded opportunities, flexibility, and enriched professional experiences. However, a thorough understanding of state regulations and clear communication are essential for successful implementation.